6:37 AM - 
 No comments
No comments

 No comments
No comments
Download 6s ECG Learner
Click Here to download 6s ECG Learner
Introduction
This guide demonstrates how to read an ECG in a systematic and effective manner.Confirm the name and date of birth of the patient matches the details on the ECG.
Confirm the date and time the ECG was performed.
Check out our ECG quiz on the new Geeky Medics quiz platform.
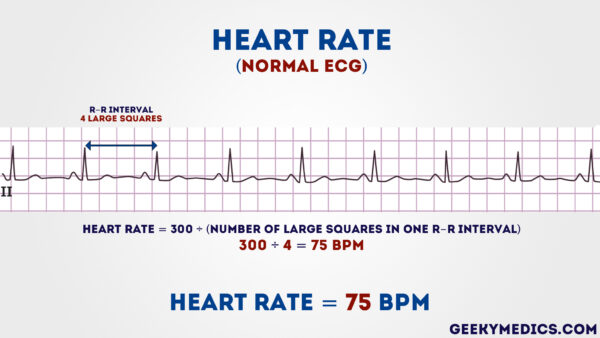
Step 1 – Heart rate
Heart rate can be calculated using the following method (if regular):- Count the number of large squares present within one R-R interval
- Divide 300 by this number to calculate the heart rate
If the rhythm is irregular:
- The
first method of calculating the heart rate doesn’t work when the R-R
interval differs significantly throughout the ECG and therefore another
method is required
- Count the number of complexes on the rhythm strip (each rhythm strip is 10 seconds long)
- Multiply the number of complexes by 6 (giving you the average number of complexes in 1 minute)
What’s a normal adult heart rate?
- Normal = 60 – 100 bpm
- Tachycardia > 100 bpm
- Bradycardia < 60 bpm
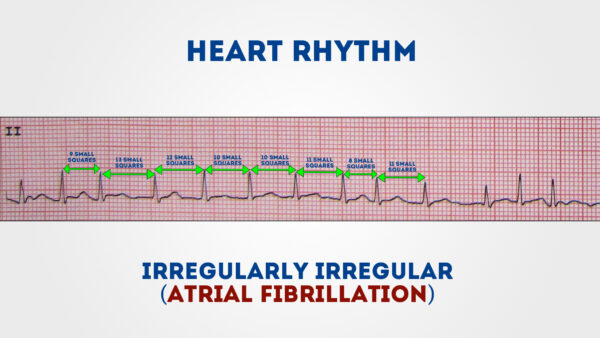
Step 2 – Heart rhythm
The heart rhythm can be regular or irregular.Irregular rhythms can be either:
- Regularly irregular (i.e. a recurrent pattern of irregularity)
- Irregularly irregular (i.e. completely disorganised)
Hint – if you are suspicious that there is some atrioventricular block, map out the atrial rate and the ventricular rhythm separately (i.e. mark the P waves and R waves). As you move along the rhythm strip, you can then see if the PR interval changes, if QRS complexes are missing or if there is complete dissociation between the two.
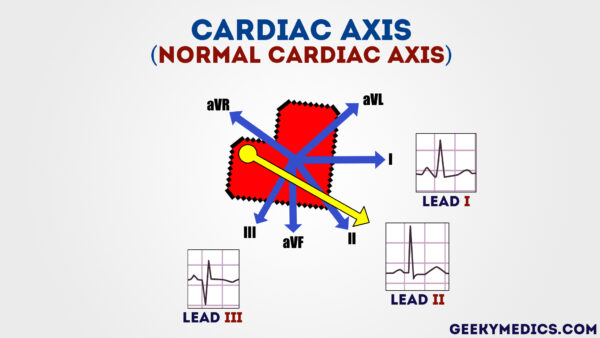
Step 3 – Cardiac axis
Cardiac axis describes the overall direction of electrical spread within the heart.In a healthy individual the axis should spread from 11 o’clock to 5 o’clock.
To determine the cardiac axis you need to look at leads I,II and III.
To get a better understanding of cardiac axis read this article.
Normal cardiac axis
In normal cardiac axis:- Lead II has the most positive deflection compared to Leads I and III
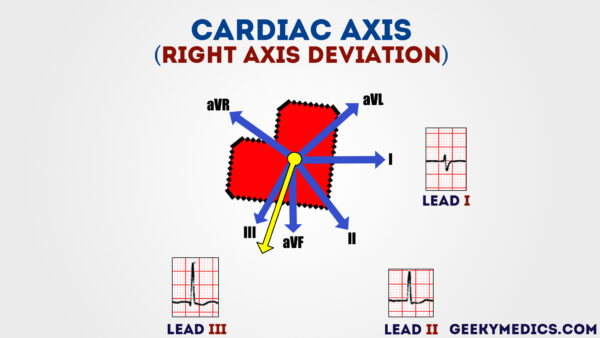
Right axis deviation
In right axis deviation:- Lead III has the most positive deflection and Lead I should be negative
- This is commonly seen in individuals with right ventricular hypertrophy
Left axis deviation
In left axis deviation:- Lead I has the most positive deflection
- Leads II and III are negative
- Left axis deviation is seen in individuals with heart conduction defects
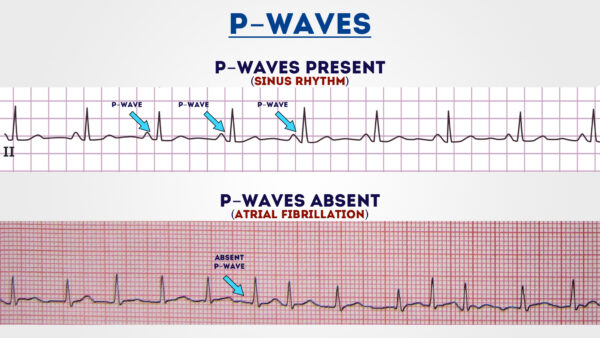
Step 4 – P-waves
Next we look at the P-waves and answer the following questions:- Are P-waves present?
- If so, is each P-wave followed by a QRS complex?
- Do the P-waves look normal? (check duration, direction and shape)
- If not present, is there any atrial activity e.g. sawtooth baseline → flutter waves / chaotic baseline → fibrillation waves / flat line → no atrial activity at all?
Step 5 – P-R interval
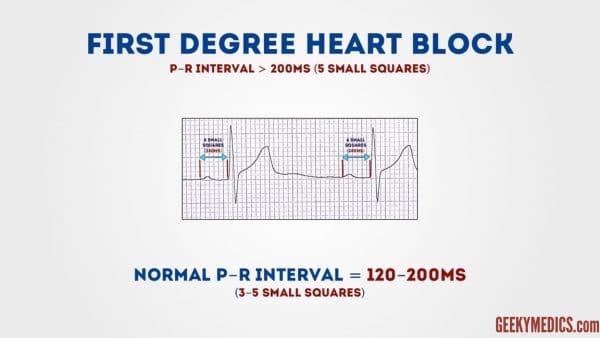
The P-R interval should be between 120-200 ms (3-5 small squares)Prolonged PR interval (>0.2 seconds)
A prolonged PR interval suggests there is atrioventricular delay (AV block)First degree heart block
First degree heart block involves a fixed prolonged PR interval (>200 ms)Second degree heart block (Mobitz type 1)
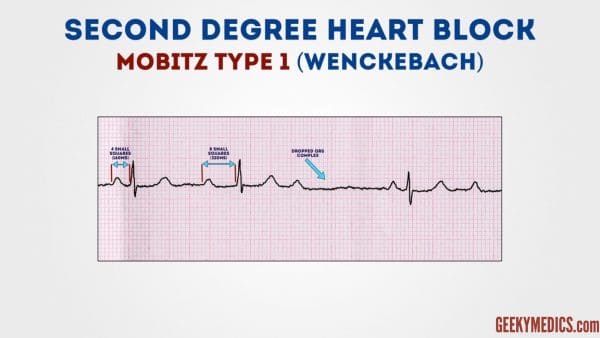
If the PR interval slowly increases then there is a dropped QRS complex (beat), this is MOBITZ TYPE I SECOND DEGREE AV BLOCK (Wenckebach)Second degree heart block (Mobitz type 2)
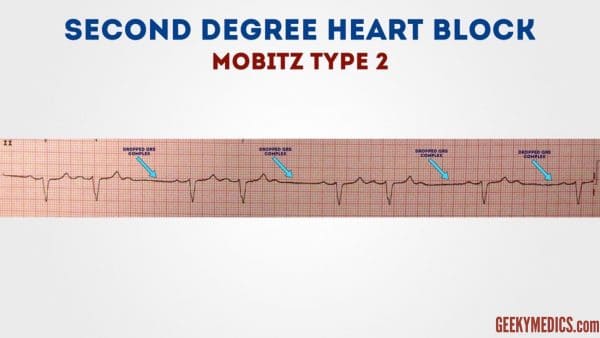
If the PR interval is fixed but there are dropped beats, this is MOBITZ TYPE 2 SECOND DEGREE HEART BLOCK (clarify that by the frequency of dropped beats e.g 2:1, 3:1, 4:1)Third degree heart block (complete heart block)
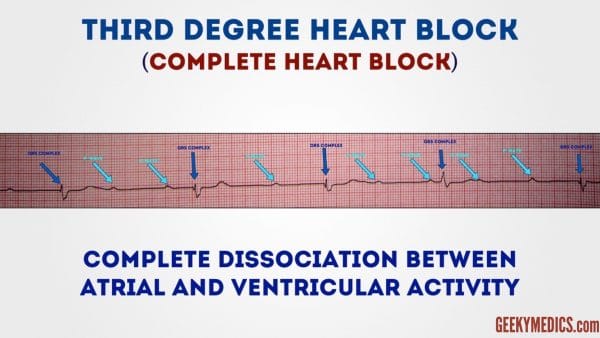
If the P waves and QRS complexes are completely unrelated, this is THIRD DEGREE AV BLOCK (complete heart block)Tips for remembering types of heart block
To help remember these degrees of AV block, it is useful to remember the anatomical location of the block in the conducting system:- First degree AV block:
- Occurs between the SA node and the AV node (i.e. within the atrium)
- Occurs between the SA node and the AV node (i.e. within the atrium)
- Second degree AV block:
- Mobitz I (Wenckebach) – occurs IN the AV node. This is the only piece of conductive tissue in the heart which exhibits the ability to conduct at different speeds
- Mobitz II – occurs AFTER the AV node in the bundle of His or Purkinje fibres
- Third degree AV block:
- Occurs anywhere from the AV node down causing complete blockage of conduction
Shortened PR interval
If the PR interval is short, this means one of two things:- Simply, the P-wave is originating from somewhere closer to the AV node so the conduction takes less time (the SA node is not in a fixed place and some people’s atria are smaller than others!)
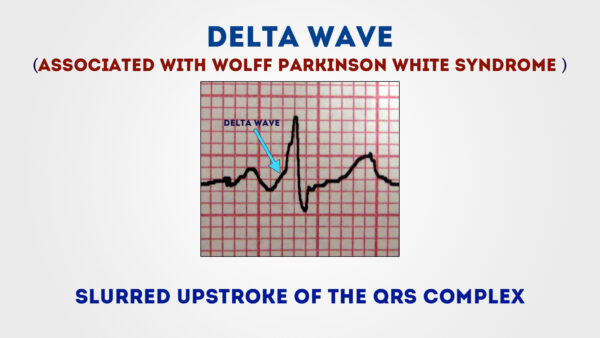
- The atrial impulse is getting to the ventricle by a faster shortcut instead of conducting slowly across the atrial wall. This is an accessory pathway and can be associated with a delta wave (see below which demonstrates an ECG of a patient with Wolff Parkinson White syndrome)
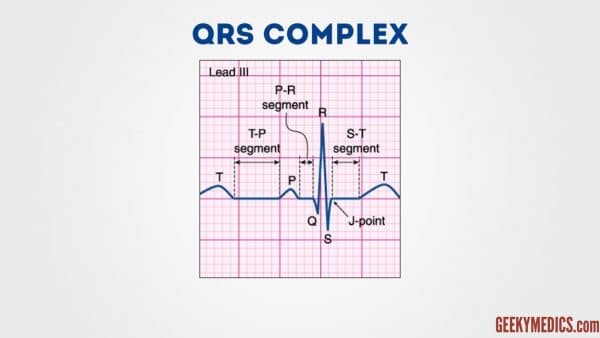
Step 6 – QRS complex
There are several aspects of the QRS complex you need to assess:- Width
- Height
- Morphology
Width
Width can be described as NARROW (< 0.12 seconds) or BROAD (> 0.12 seconds)- A narrow QRS complex occurs when the impulse is conducted down the bundle of His and the Purkinje fibre to the ventricles. This results in well organised synchronised ventricular depolarisation.
- A broad QRS complex occurs if there is an abnormal depolarisation sequence – for example, a ventricular ectopic where the impulse spreads slowly across the myocardium from the focus in the ventricle. In contrast, an atrial ectopic would result in a narrow QRS complex because it would conduct down the normal conduction system of the heart. Similarly, a bundle branch block results in a broad QRS because the impulse gets to one ventricle rapidly down the intrinsic conduction system then has to spread slowly across the myocardium to the other ventricle.
Height
Describe this as SMALL or TALL:- Small complexes are defined as < 5mm in the limb leads or < 10 mm in the chest leads.
- Tall complexes imply ventricular hypertrophy (although can be due to body habitus e.g. tall slim people). There are numerous algorithms for measuring LVH, such as the Sokolow-Lyon index or the Cornell index.
Morphology
You need to assess the individual waves of the QRS complex.Delta wave
The mythical ‘delta wave’ is a sign that the ventricles are being activated earlier than normal from a point distant to the AV node. The early activation then spreads slowly across the myocardium causing the slurred upstroke of the QRS complex. Note – the presence of a delta wave does NOT diagnose Wolff-Parkinson-White syndrome. This requires evidence of tachyarrhythmias AND a delta wave.Q-waves
Isolated Q waves can be normal. A pathological Q wave is > 25% the size of the R wave that follows it or > 2mm in height and > 40ms in width. A single Q wave is not a cause for concern – look for Q waves in an entire territory (anterior / inferior) for evidence of previous MI.R and S waves
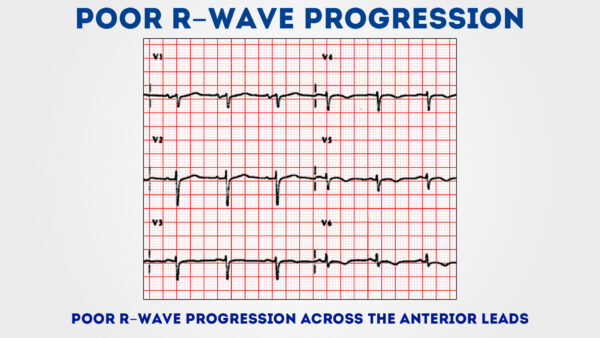
Look for R wave progression across the chest leads (from small in V1 to large in V6). The transition from S > R wave to R > S wave should occur in V3 or V4. Poor progression (i.e. S > R through to leads V5 and V6) can be a sign of previous MI but can also occur in very large people due to lead position.J point segment
The J point is where the S wave joins the ST segmentThis point can be elevated resulting in the ST segment that follows it also being raised (this is known as “High take off”)
High take off (or benign early repolarisation to give its full title) is a normal variant that causes a lot of angst and confusion as it LOOKS like ST elevation
Key points:
- Benign early repolarisation occurs mostly under the age of 50 (over age of 50, ischaemia is more common and should be suspected first)
- Typically, the J point is raised with widespread ST elevation in multiple territories making ischaemia less likely
- The T waves are also raised (in contrast to a STEMI where the T wave remains the same size and the ST segment is raised)
- The changes do not change! During a STEMI, the changes will evolve – in benign early repolarisation, they will remain the same.
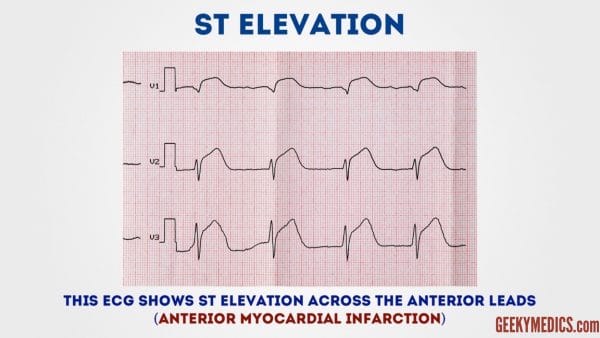
Step 7 – ST segment
The ST segment is the part of the ECG between the end of the S wave and start of the T wave.In a healthy individual it should be an isoelectric line (neither elevated or depressed).
Abnormalities of the ST segment should be investigated to rule out pathology.
ST elevation
ST elevation is significant when it is greater than 1 mm (1 small square) in 2 or more contiguous limb leads or >2mm in 2 or more chest leads.It is most commonly caused by acute full thickness myocardial infarction.
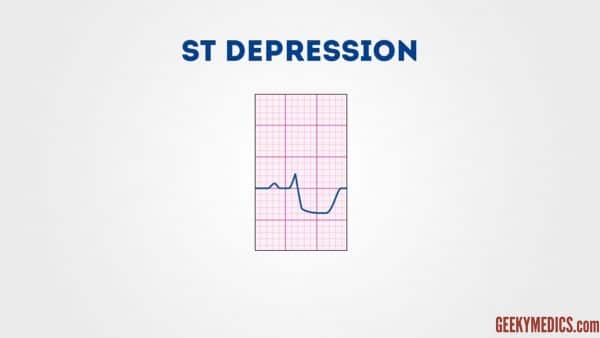
ST depression
ST depression ≥ 0.5 mm in ≥ 2 contiguous leads indicates myocardial ischaemia.Step 8 – T waves
The T waves represent repolarisation of the ventriclesTall T waves
T waves are tall if they are:- > 5mm in the limb leads AND
- > 10mm in the chest leads (the same criteria as ‘small’ QRS complexes)
Tall T waves can be associated with:
- Hyperkalaemia (“Tall tented T waves”)
- Hyperacute STEMI
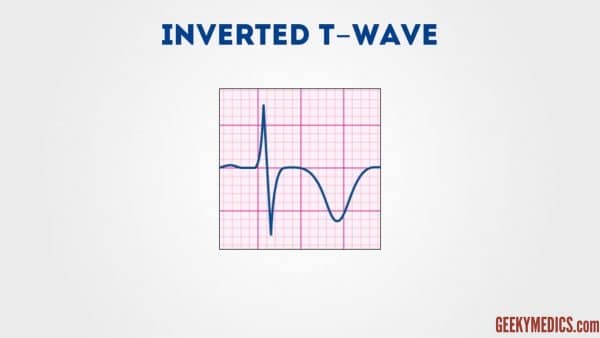
Inverted T waves
T waves are normally inverted in V1 and inversion in lead III is a normal variant.Inverted T waves in other leads are a nonspecific sign of a wide variety of conditions:
- Ischaemia
- Bundle branch blocks (V4 – 6 in LBBB and V1 – V3 in RBBB)
- Pulmonary embolism
- Left ventricular hypertrophy (in the lateral leads)
- Hypertrophic cardiomyopathy (widespread)
- General illness
Comment on the distribution of the T wave inversion e.g. anterior / lateral / posterior leads
You must take this ECG finding and apply it in the context of your patient
Biphasic T waves
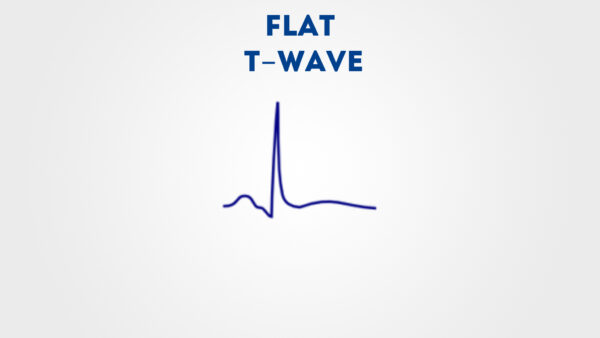
Biphasic T waves have two peaks and can be indicative of ischaemia and hypokalaemiaFlattened T waves
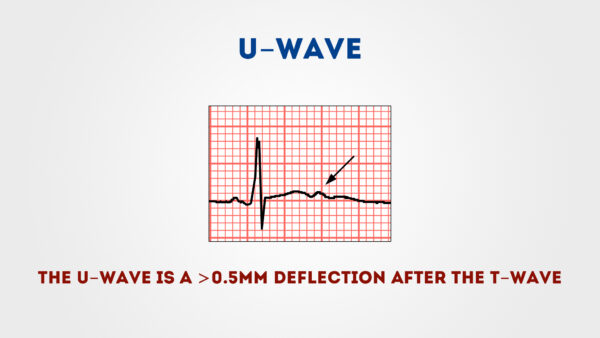
Another non-specific sign, this may represent ischaemia or electrolyte imbalance.U waves
Not a common finding.The U wave is a > 0.5mm deflection after the T wave best seen in V2 or V3.
These become larger the slower the bradycardia – classically U waves are seen in various electrolyte imbalances or hypothermia, or antiarrhythmic therapy (such as digoxin, procainamide or amiodarone).